JIA
-
disease onset before age 16, and
-
joint pain not caused by a known infectious-, inflammatory-, or haemato-oncologic disease.
Doctors distinguish between different types of JIA based on symptoms during the first six months of the disease.
Systemic JIA
Previously called Stills Disease, in addition to joint pain, sJIA is noted for high spiking fevers and a salmon-colored rash. The prognosis is very good.
Oligoarticular JIA
Previously called pauciarticular JRA, this type of JIA involves fewer than five joints during the first six months of disease. If this continues past six months it is called persistent oligoarticular JIA; if joint involvement increases to five or more after the intitial six-months of disease it is called extended oligoarticular JIA. Half of all JIA diagnoses are for oligoarticular JIA.
Polyarticular JIA
This form of JIA is subdivided into two groups depending on whether or not lab tests are positive for rheumatoid factor.
RF+ is sometimes called sero-positive. It is considered the juvenile version of adult RA. Less than five percent of JIA diagnoses are for this form of the disease.
RF– is sometimes called seronegative. Other than that, symptoms are like the seropositive form of the disease.
Psoriatic JIA
Diagnosis of PsJIA can be challenging because it is possible for a child to have Psoriatic Arthritis without having any skin symptoms of psoriasis.
Enthesitis Related Arthritis (ERA-JIA)
Enthesitis is part of the spondyloarthropathy family, a family of autoimmune diseases that are more likely to affect the spine than other types of JIA.
Undifferentiated JIA
Sometimes children definitely have a type of inflammatory arthritis, but do not meet the diagnostic criteria of one of the other forms of JIA. Other times children appear to meet the diagnostic criteria of more than one type of JIA. In these cases, doctors say that the disease hasn’t declared (differentiated) itself yet, and the diagnosis is Undifferentiated JIA.
It is likely that the naming system will change again as new research reveals more about these autoimmune diseases.
People who receive a diagnosis of one of the forms of JIA do not receive a different diagnosis when they become adults. The diagnosis remains JIA, even if the person lives to be 80 years old.
Incidence – In studying juvenile idiopathic arthritis, epidemiologists1 have learned that for every 100,000 children, there are between 1-22 new cases of JIA diagnosed annually – this is the incidence of JIA.
Prevalence – For every 100,000 children, there are 8-150 people dealing with JIA on an ongoing basis (prevalence). JIA has such a low prevalence that it is considered a rare disease by Orphanet.
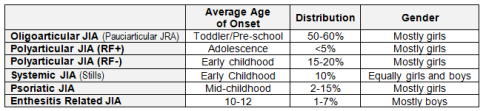
Age of Onset – Age of onset varies depending on the subtype of JIA. About half of the cases of JIA are oligoarticular JIA, which is most commonly diagnosed in 1-3 year old girls. Systemic JIA and seronegative polyarticular JIA are typically diagnosed in early childhood, while psoriatic JIA tends to be diagnosed in mid-childhood. ERA is usually diagnosed in boys aged 9 and up. Girls with seropositive polyarticular JIA are usually diagnosed during adolescence. These are, however, averages, and not rules. JIA is rare in babies younger than 6 months, but it does occur. Immune systems don’t read textbooks, thus any of these diseases can occur in boys and girls of any age.
Sources:
JIA: Epidemiology and Immunopathogenesis
Juvenile Arthritis in the Classroom
__________
1Epidemiology is the study of health and disease patterns. What causes a specific disease? How does it spread? How many people are newly diagnosed in a year? How many people are managing the disease on an ongoing basis?
You might also hear the term Juvenile Rheumatoid Arthritis. You can read about the distinction between JRA and JIA here.